Ultrasound examination
Ultrasound examination is the best way to determine the shape, size and position of the uterus. Advantages are that it is informative and comforting for the woman. With ultrasound one measures the probe length of the uterus. It will not be necessary to measure with a uterine sound during insertion.
Bimanual examination
If no ultrasound is available it is necessary to perform a bimanual examination to determine the shape, size and the position of the uterus, this can cause some discomfort. We advise women to take an ibuprofen or 2 paracetamol 30 minutes before insertion.
A uterine sound is used to measure the length of the uterus.
Visualizing and cleaning the cervix
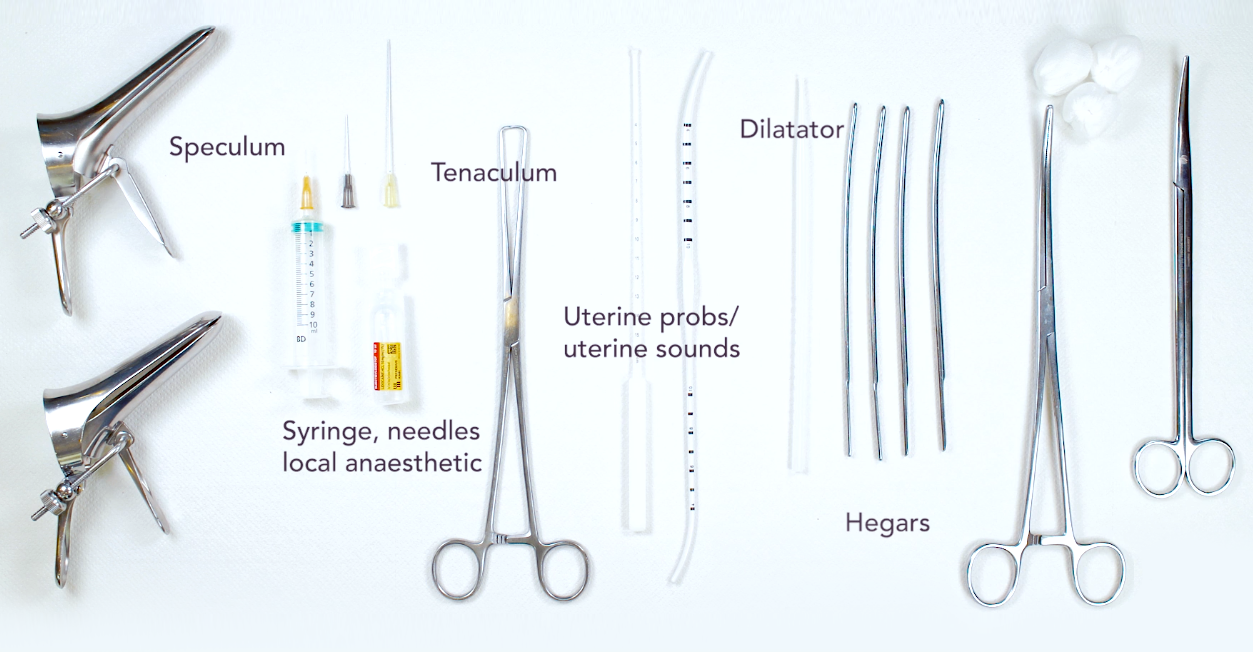
Setting up the portio requires a speculum. Use a self-containing speculum. This way you will be able to use both hands. Specula come in different shapes and sizes. The distance to the cervix determines which speculum is best. Preferably you pick a speculum with the shortest possible length. Advantage is that it will be easier to stretch the cervix before insertion. A speculum of the wrong size makes insertion more difficult or sometimes even impossible.
Start to disinfect the cervix with an antiseptic solution
Local anaesthetics
Please note that local anaesthetics are optional and not available in every country.
To administer a local anaesthetics it’s preferable to use a 10cc syringe. This syringe, together with a short needle, has enough length to reach the cervix. Take 2cc of an anaesthetic, for example lidocaine. Place the needle against the cervix a couple of mm above the external os and give a short tap to insert the needle. If this happens too slowly you will only push the cervix away. Inject about half a mm, which results most of the time in whitening of the injection area. If the cervix is large, inject 2 or three areas. Always inject where you want to place the tenaculum.
Grasping the cervix
The next step is to fix a tenaculum to the cervix. Position the tenaculum with care and policy just above the external orifice.
Close the tenaculum by just fixing it to the cervix. Usually it is not necessary to close it completely. Complete closure will cause more discomfort and pain for the woman.
Dilation
To prevent a Flexi T from bending or turning during the insertion trying to pass the external and internal orifice you should use a dilator/ hegar(s). This simplifies the insertion because it enlarges the tissue temporarily. With the help of hegars the internal orifice can be stretched with steps of half a millimetre.
In case the internal orifice can be passed, it is also possible to place the Flexi-T. It is not necessary that a dilator has a size indication.
Before you insert the dilator, carefully pull the tenaculum so that the uterus stretches. Sometimes it is necessary to pull the speculum back slightly.
After measuring the sound length and dilation for easy insertion, you take out the FlexiT, holding it at the end of the inserter tube. You put the blue ring in the correct measured sound distance. The blue thread will come loose. Fix the blue thread between thumb and forefinger on the insertion tube. This will make sure that the Flexi-T is fixated against the insertion tube. The Flexi-T will stay well in position and this makes it easier to insert. If you do not hold the blue thread, the Flexi-T can turn around during insertion or fall out of the tube.
An experienced gynaecologist can feel when the IUD has reached the fundus, the blue ring is not always necessary. Make sure that the blue thread is loose.
Ultrasound/ bimanual check
Check with an ultrasound whether the IUD is in the correct position in the uterus. The woman can also see this herself. If no ultrasound is available gently pull on the thread protruding from the inserter tube in order to check whether the arms are unfolded and the device is held by the lateral muscular wall of the uterus.
After this check has been performed, gently push the inserter tube with the device again towards the fundus, make sure the blue thread is loose.
Bimanual examination
If no ultrasound is available it is necessary to perform a bimanual examination to determine the shape, size and the position of the uterus, this can cause some discomfort. We advise women to take an ibuprofen or 2 paracetamol 30 minutes before insertion.
A uterine sound is used to measure the length of the uterus.
Removing the insertion tube
Start with removing the tenaculum
Remove the inserter tube cautiously using a rotating movement in order to prevent the Flexi-T being pulled downwards or out.
Cutting the wire
When you take out the inserter tube, do not remove the entire tube. This way you can easily cut the wire. The wire is cut at 1.5 cm. Then the speculum is removed.
Care after insertion
A vaso-vagal reaction may occur due to stimulation of the vagus nerve when dilating the internal orifice. This is more common in nulliparous women. Knowledge and control of the vasal vagal reaction are necessary to properly monitor and assist the patient.
Check 4 -6 weeks
The presence and position of the Flexi-T should be verified at least after the first cycle and after ± six months. Although self-examination is possible to a limited extend it may not provide the correct information,
Skilful professionals contribute to happy women with safe contraception.
